"Knee replacement" is surgery in which a layer of bone is removed from all three knee bones of the knee. The removed layer is then replaced with artificial material, namely metal and plastic.
The operation is performed using battery-powered saws, chisels, hammers, etc. This operation is often called "full knee replacement," or "total knee arthroplasty." Despite the name, it obviously is not a replacement of the entire human knee.
The bone model below demonstrates a left knee replacement; the kneecap is not shown. To the left is the intact femur and tibia. The middle picture shows appearance after removal of the diseased bone. To the right, the bone ends are covered with the artificial prosthesis.

The knee joint
Three bones meet at the knee joint.
- The femur starts above at the hip and ends as the upper bone at the knee.
- The tibia starts at the knee, and ends at the ankle.
- The patella, the kneecap, is part of the quadriceps muscle mechanism; it serves to transmits the quadriceps muscle forces to the tibia, so that one may be able to straighten the knee, climb stairs, stand from squatting, etc.
Is there more than one kind of knee replacement?
Yes. Below a few variations on the theme.
- UKA, unicompartment knee arthroplasty, or partial knee replacement is appropriate for patients with anteromedial osteoarthritis. UKA is a better operation than the full knee replacement for these patients.
- TKA, total knee arthroplasty; this is what is usually meant by "knee replacement". In the US, traditionally the operation involves resurfacing of the patella as well.
- PS, posterior substituting. This refers to a type of TKA prosthesis. This is a design philosophy for knee replacement prostheses that does away with the need to have a functional PCL (posterior cruciate ligament).
- CR, cruciate retaining. This is the other type of knee replacement prosthesis.
- Cemented vs uncemented knee replacement: most surgeons use PMMA to fix the artificial parts to the bone.
- The terms computerized, navigated, prenavigated, PSI, Mako, robotic, etc., refer to certain tools and methods that the surgeon may use to help measure and make the bone cuts. The fundamental nature of the operation does not change.
- Last but not least: there are many manufacturers of knee replacement prostheses. The "big 3" of the knee prostheses are Zimmer, DePuy, and Stryker. Each of these manufacturers offers more than one different model. The situation is similar to the car market, where there is an abundance of choices, each with its own advantages and drawbacks.
What is the best method for replacing a knee?
There are thousands of scholarly papers on the topic, which often contradict each other, or are just somebody's opinion or bias (as opposed to accepted truth). Nobody can say for sure. The joint arthroplasty registries from the socialized medical systems of Europe provide some of the best data to help one decide what is good and what is not so good.
Based on my review of literature and my own extensive experience, for routine knee replacements I typically use the following
- Standard medial para-patellar arthrotomy.
- Cemented Zimmer Persona MBC prosthesis.
- Intramedullary rod alignment for the femur, extramedullary for the tibia.
- I use cement, loaded with antibiotic, every time.
- Meticulous wound closure.
However, I recognize that there are other ways to do a good knee replacement. In particular, for patients who request it, I offer the robotic replacement with the Mako/Stryker prosthesis. All you have to do is ask.
Why not do the robotic knee replacement for everybody?
- Studies show it does not result in better outcomes. This should be reason enough.
- Robotic replacement requires an additional CT before surgery.
- Robotic surgery requires placement of additional metal pins in the bone during surgery, in order to allow the computerized equipment to "know" where the bone is.
Typical course after a knee replacement operation
- I perform this operation with spinal anesthesia.
- Patients usually go home the same day or next day.
- Immediate weight bearing.
- Physical therapy in hospital:
- full extension
- at least 90 degrees of flexion
- walking with walker starting immediately.
- Physical therapy after discharge must continue without interruption.
- Follow up at
- 2 weeks after surgery for staple removal
- 6 weeks after surgery
- 3 months, 6 months, and 12 months after surgery
- Expect to discontinue walker at 3 weeks.
- Most patients are able to walk comfortably by 6 weeks.
- The knee can be warm and can look swollen for 1 year after surgery.
- The best predictor of post-operative flexion is preoperative flexion. Multiple statistical studies have shown this, and it is not realistic to expect to bend the knee fully after surgery, if you could only bend the knee 45 degrees before surgery.
- The ability to kneel down is affected by total knee replacement. This is a limitation of current technology.
- I no longer routinely advise antibiotics for dental procedures after knee replacement. There is not medical evidence to support antibiotic use before dental procedures in patients with otherwise good oral health.
Risks of knee replacement
Knee replacement is a routine operation, but it is a violent operation during which motorized power tools and heavy hammers are used. It is not risk free and complications can occur.
Here is a list:
- Death. A heart attack can be brought on by anxiety before or after, by blood loss, by pain, by a blood clot.
- Infection. On average, in the US there is 1 infection for every 100 of these operations. Infection after TKA is a most serious complication. It is often necessary to remove the knee replacement, try to cure the infection, and then reinsert a prosthesis at a later date. Infection, in the best case scenario, makes for a very bad 6 months or so. Even when the infection is finally cured, the outcome expected is less than it would have been without an infection. Unfortunately, there is no sure way to prevent an infection.
- Amputation, limb loss. It happens very rarely in the US, the culprit is usually infection.
- DVT and PE. 1-2 % of patients suffer from this complication.
- Loosening and wear of the prosthesis.
- In 100% of the cases, there is some numbness from the incision and sacrificing of the infra patellar branch of the saphenous nerve.
- On rare occasions there may be temporary numbness and ankle paralysis from stretching of the peroneal nerve. Foot paralysis after TKA is very much possible and has been described in literature.
- Across the US, statistics show that approximately 15% of patients who receive knee replacements are not entirely happy with them for one reason or another.
How long does a knee replacement last?
10 and 15 year survival rates are approximately 95% and 90% respectively. This means that out of 100 implanted prostheses, 15 years later 10 of those prostheses have failed for various reasons, including infection, mechanical wear, loosening, fracture, etc.
What happens when a prosthesis fails?
Depends on the reason of failure. Most times it is possible to do revision surgery and reinsert a new part, or a whole new prosthesis.
How is knee arthritis diagnosed?
Knee arthritis is diagnosed by xray. An MRI typically not necessary. It is an unnecessary expense of time and treasure, and should be avoided. (There are, of course, individual circumstances and exceptions.)
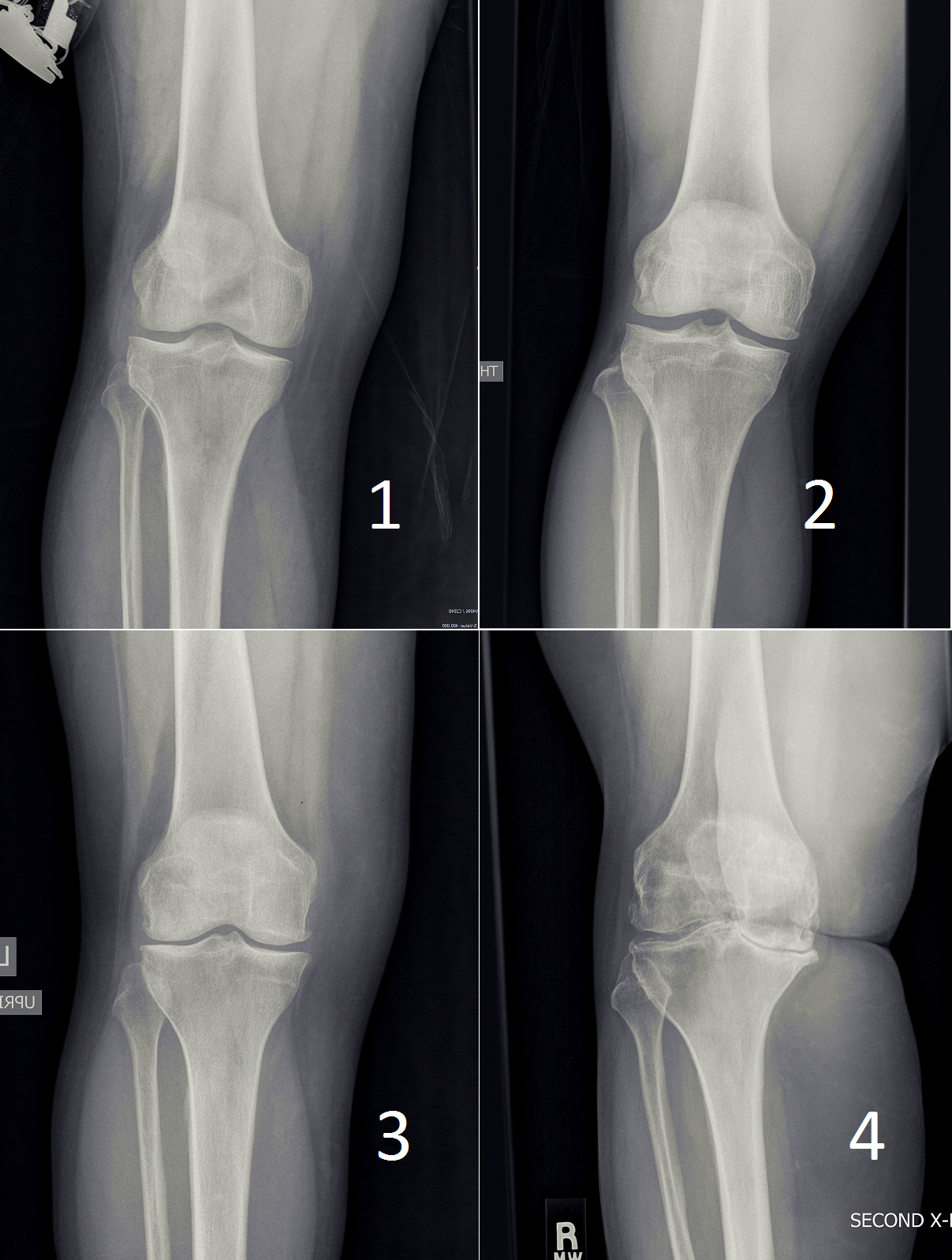
The following picture shows xrays of patients with different grades of arthritic disease. Grade 1, the mildest, has "doubtful" findings on xray. At the other end of the spectrum grade 4 has "bone-on-bone" disease, deformity, large osteophytes, and so on.
Is there a way to stop arthritis and avoid knee replacement?
At this particular moment in time, in the year 2025AD, if a knee joint has become arthritic, there is no way to stop or reverse the process. Arthritis is progressive, and tends to get worse with time. This sounds hopeless, but in reality it is no worse than many other human ailments. On the positive side, treatment and pain relief is possible.
Are there alternatives to knee replacement?
If the disease is not severe, non-surgical option should be attempted first
- If pain is tolerable, no specific knee intervention is needed.
- "Activity modification": this implies doing less of whatever it is that makes the knee hurt.
- NSAID medications: if Tylenol does not help, it is worth trying naproxen, or ibuprofen, or mobic.
- Needle aspiration of knee effusions and judicious use injections oftentimes help tremendously, but of course, they do not stop the disease.
- Arthroscopic surgery:
- Unfortunately, arthroscopy is not very effective for knee arthritis. Unless there is a specific treatable issue such as a loose body, or a large meniscal tear that acts as a loose body, or some other such problem, you can expect arthroscopy to not help a lot with the arthritic pain. Understanding that it probably won't solve the problem, one may still wish to try arthroscopic surgery because it is a much smaller operation.
Case study
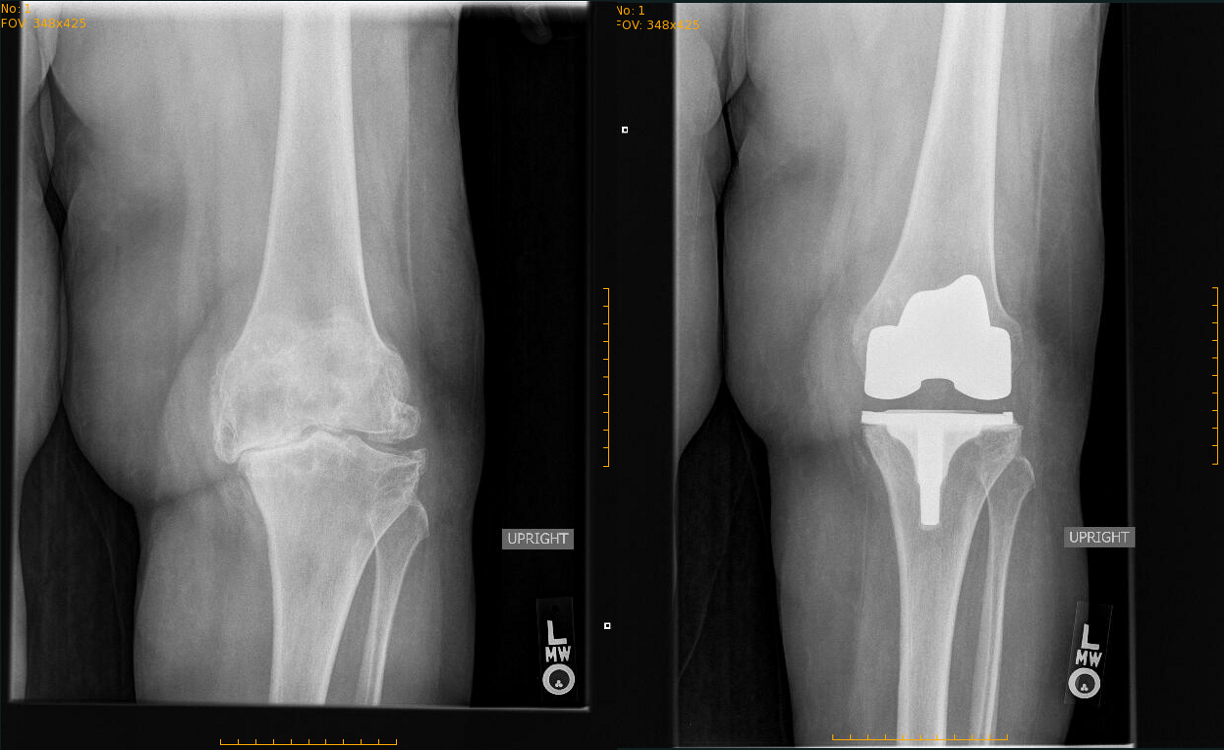
Before and after pictures of a knee replacement of a very arthritic knee that I treated with knee replacement.